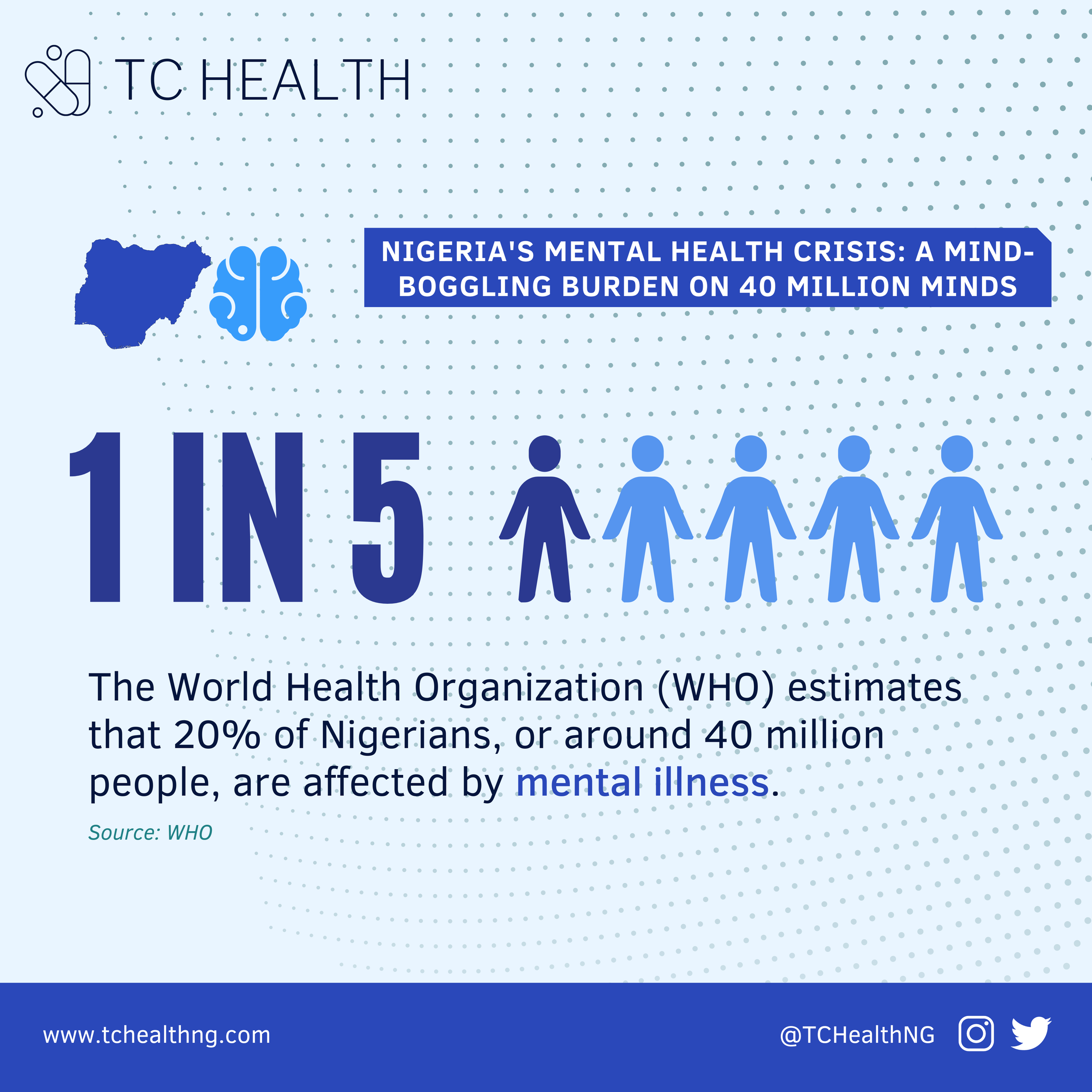
Nigeria's Mental Health Crisis: A Mind-Boggling Burden on 40 Million Minds
Nigeria is grappling with a staggering mental health crisis, as millions of its citizens suffer from various mental disorders. The World Health Organization (WHO) estimates that a whopping 20% of Nigerians, or around 40 million people, are affected by mental illness.
Some of Nigeria's most prevalent mental illnesses include depression and anxiety disorders. In 2017, about 7 million Nigerians (3.9% of the population) had depressive disorders, and 4.9 million Nigerians (2.7%) had anxiety disorders. On top of this, substance abuse disorders, bipolar disorder, schizophrenia, and personality disorders are common in Nigeria.
The burden of illness related to post-traumatic stress disorder (PTSD) and other trauma-related disorders is also significant, particularly among individuals who have experienced conflict, violence, or natural disasters. Studies have shown that close to 60% of internally displaced persons (IDPs) in Kaduna had probable depression, and 16% had definite depression.
Mental illnesses have a significant, real-life impact on many Nigerians. The impact of these illnesses extends beyond the individual, with healthcare workers, teachers, and even bankers also affected. Studies have found that psychological distress and burnout are prevalent among healthcare workers and primary school teachers, with almost 70% of teachers experiencing psychological distress. Additionally, the psychological health of bankers has been linked to corruption and unethical behavior, which is detrimental to banks' performance and growth.
Despite Nigeria's huge mental illness burden, the country faces severe challenges in addressing the problem.
The most pressing issue is the country's shortage of mental health professionals. Currently, only about 200 psychiatrists and 1000 psychiatric nurses serve over 200 million people in Nigeria, whereas the standard practice is for one psychiatric doctor to care for 10,000 patients. Beyond psychiatrists, there is also a shortage of psychologists in the country. Psychologists are key professionals in providing services for people with mental conditions such as behavioural problems, learning difficulties, depression, and anxiety. Currently, there are only 319 licensed clinical psychologists that are registered with the Nigerian Association of Clinical Psychologists (NACP); however, estimates suggest that there could be 400-500 clinical psychologists in Nigeria. There are several discrepancies in the level of qualifications among clinical psychologists in the country - some have received online training or a 6-month certification program, while others have acquired a professional doctorate - making it difficult to know the true number of certified and experienced clinical psychologists. Nonetheless, these numbers are alarming statistics for the country’s considerable population.
According to the president of the Association of Psychiatrists in Nigeria (APN), Professor Taiwo Obindo, the brain drain of mental health professionals to Western countries such as the US and the UK is a major factor in this shortage. He revealed that up to two-thirds of well-trained and certified psychiatric doctors leave the country annually.
The Federal Neuro-Psychiatric Hospital Yaba, Lagos, is one of the most indicative case studies of these challenges. Financial deficits and other challenges have caused the Yaba Hospital to lose half of its resident psychiatrists over the past four years, leaving only 33 resident doctors and 22 consultants to address the needs of more than 5,000 patients treated each year.
Comparing statistics with other Sub-Saharan African countries reveals the scale of the issue on the continent - Kenya has only about 80 psychiatrists and 30 clinical psychologists, South Africa boasts 22 psychiatric hospitals and 36 psychiatric wards, and Ghana has three psychiatric hospitals and about 20 psychiatrists.
The situation is further compounded by cultural barriers and stigma surrounding mental health. Other healthcare professionals look down on mental health professionals due to this stigma; as a result, psychiatrists are usually a last resort for very dire patients. Additionally, patients are typically referred to behavioral and clinical/counseling psychologists when it's too late, oftentimes after seeing and receiving medical treatment from psychiatrists.
Insights from the general Nigerian population are even more telling of the severe stigma faced by people living with mental disorders. According to a survey of over 5,000 Nigerians conducted in 2020, many Nigerians only perceive a person as having a mental health disorder when disruptive behavior attracts public attention. This stigma is also evident in romantic relationships, with most Nigerians, especially females, unwilling to engage in relationships with people living with mental health disorders.
Additionally, the general population often seeks treatment from traditional and supernatural healers, given the predominant view of supernatural causation. Approximately 70% of mental health treatment is provided through non-orthodox means. Respondents believe mental health diseases can be prevented if people stop taking hard drugs and are prayerful. Many believe that a mental health disorder is a curse from God or punishment for the victim's wrongdoing.
Another significant issue is Nigeria's lack of access to mental health services. The funding for mental health care is limited, with only a small fraction of the central government health budget (3-4%) dedicated to mental health. On top of that, over 90% of this budget goes to a handful of neuropsychiatric hospitals, leaving few resources for other facilities. In the private sector, the story isn’t very different. Health Maintenance Organizations (HMOs), which provide health insurance coverage primarily through employer-sponsored programs, are also not providing adequate mental health benefits. While some plans include mental health benefits, these primarily consist of psychiatry services that do not cover the much-needed behavioral therapy for those suffering from anxiety and depression.
Access to mental health services in Nigeria is a significant issue, but it is not unique to the country. Other sub-Saharan African countries also struggle with limited access to mental health care. In Ghana, for example, 97% of mental patients who need health care have no access to these services. Around 75% of people with mental illnesses in South Africa have no access to psychiatric or therapeutic care. The National Health Insurance program in South Africa, which could potentially boost access to mental health care, will not be fully implemented until at least 2025. Similarly, according to the World Health Organization, Kenya spends only about 0.05% of its budget on mental health.
So it has already been established that mental health service delivery and access in Nigeria desperately need improvement, but what can be done about this? Several solutions can be explored to improve the current state of mental health in Nigeria.
For instance, employers taking a more active role in promoting mental health could alleviate some of the burdens within the Nigerian workforce. This can be done by integrating mental health into their employees' benefits, particularly in the post-COVID world. Studies have shown that mental health problems account for 7.1% of workplace absenteeism and $4.5 billion in work-related productivity losses, making it an important issue for human resource managers. Employers can take steps to ensure both physical and mental health is promoted, which will ultimately lead to a more productive workforce.
It is also important to integrate mental health into primary healthcare in Nigeria. This will help improve access to and affordability of mental health services. Many countries, such as Argentina, Australia, and the United Kingdom, have already recognized the importance of mental health as part of primary care, resulting in better health outcomes. Research has shown that one way to achieve this in Nigeria is to establish community-based rehabilitation centers in rural areas with strong primary care networks. These centers can provide complementary care and work closely with secondary and tertiary care centers. The centers can also serve as training sites for psychiatric residents, primary care physicians, and nurses.
On the topic of training, reversing the brain drain for psychiatrists and psychologists in the country is key to unlocking better mental health service delivery. There is a need to establish more training institutions and programs for mental health professionals in Nigeria. Partnerships with societies such as the Association of Psychiatrists in Nigeria (APN) and the Nigerian Society of Clinical Psychologists could be leveraged to provide these training opportunities. This will address the shortage of mental health specialists in the country and improve the overall quality of mental healthcare in Nigeria.
Without adequate funding, implementing any of the solutions discussed would be impossible. It is crucial for the government to increase the allocation of funds from health budgets to improve the accessibility, quality, and affordability of mental health services in Nigeria. With more resources, it will be possible to establish additional rehabilitation centers and train more mental health professionals, thus improving access to quality care and support for those in need.
In the private sector, some companies are trying to bridge the gap in access and provision of mental health services in Nigeria. Akoma Health is a startup that provides access to quality, on-demand therapy and support for Nigerians. Akoma is actively exploring partnerships with psychiatry and psychology professional societies to expand the supply of their HCPs within their network and integrate their services with HMOs and employers to improve access to mental health services for their members.
Akoma recently partnered with Lagoon Hospitals, one of the largest hospital networks in Nigeria, to provide teletherapy mental healthcare support to all of Lagoon’s private and corporate clients. This partnership enables direct access to Akoma’s highly-trained and licensed support team of clinical psychologists and mental health professionals on its digital platform.
Key Takeaways from TC Health: Nigeria's mental health care system requires urgent improvement. Employers, healthcare providers, and the government should collaborate to integrate mental health care into primary healthcare, establish more mental health training institutions, and increase funding for mental health services. With the current macroeconomic and political pressures and the impact of the pandemic on the workforce and population, prioritizing the mental health of Nigerians has never been more critical. These solutions are necessary for a healthy population and must be made a reality.